
Management of relapsed follicular lymphoma
Introduction
Follicular lymphoma (FL) is the second most common subtype of non-Hodgkin lymphoma (NHL), accounting for nearly 14,000 new diagnoses every year in the United States (1). Current conventional therapy is not thought to curative, though due to expanding disease knowledge and growing therapeutics, most patients experience a prolonged overall survival (OS) exceeding twenty years (2). Due to its usual indolent course, treatment of FL is not always needed at the time of diagnosis. Instead, most clinicians recommend delaying therapy until the arrival of progressive disease or advancing symptoms (3). That being said, FL is a heterogeneous disease and can have a varied clinical course depending on disease biology and patient characteristics. For these reasons, initial treatment regimens are tailored to the patient and their unique situation, including patient age, comorbid conditions, and disease risk stratification [such as the Follicular Lymphoma International Prognostic Index (FLIPI)]. The same is valid for treatment considerations in the relapsed and refractory settings.
FL is typically very responsive in the upfront setting, with complete response (CR) rates exceeding 70% (4-7). Refractory disease with initial chemoimmunotherapy is rare, occurring in less than 10% of patients (7). Unfortunately, most FL patients will experience disease relapse, though usually after a prolonged progression-free survival (PFS) with initial therapy. When a patient experiences a disease relapse, multiple factors must be weighed. A biopsy should also be considered as transformed large cell lymphoma occurs in around 2–3% of patients per year and roughly 30% of patients with FL by ten years after their diagnosis (8,9).
Additionally, accurate FL grading is crucial as transformed FL and grade 3b FL are treated differently than grade 1-3a FL. Further risk stratification has also been implemented through scoring systems such as FLIPI and understanding the importance of time to relapse. Patients with early relapsing FL, often defined as disease progression within 24 months (POD24), have worse clinical outcomes compared to those patients who do not experience disease relapse in 2 years. Nearly 20% of patients treated with chemoimmunotherapy will experience POD24 (10). POD24 remains an unmet need in FL and will be covered separately due to its high-risk nature. Finally, patient age, comorbid conditions, prior treatment, and treatment goals should be accounted for when forming a treatment plan that addresses disease biology and individual patient preferences.
This section will outline management paradigms in relapsed FL, including agents currently approved and those under investigation in clinical trials. Treatments range from conventional chemoimmunotherapy to cellular options such as stem cell transplantation, in addition to novel agents. As patients with FL live longer, expanding knowledge of relapsed disease is critical, including an improved understanding of disease heterogeneity and risk stratification.
Consideration of treatment
Before initiating therapy, it is critical to confirm the nature of disease relapse. As stated previously, transformed disease is treated similarly to diffuse large B-cell lymphoma (DLBCL). It can be suspected with rapidly progressive symptoms, high lactate dehydrogenase (LDH), and areas of intense fluorodeoxyglucose (FDG) PET avidity (11). A biopsy is often indicated to confirm relapse with non-transformed disease. Once disease relapse with FL has been established, the initial decision is whether treatment is necessary. In non-transformed disease and those without POD24, active observation can be considered in patients with slow disease tempo and low tumor burden (3).
If treatment is needed, a range of options exist from single-agent anti-CD20 monoclonal antibody therapy to high-dose salvage chemotherapy and an autologous stem cell transplant (ASCT). The precise sequencing of treatment is not known. Instead, clinical judgment must be used, considering disease tempo, patient preference, and available clinical data. Most patients will experience multiple relapses throughout their life, thus treatment decisions will vary depending on the treatment history. Conventional and investigational agents will be covered in the subsequent sections through the lens of common clinical scenarios to understand the range of available options.
Clinical scenario 1
An 82-year-old man presents for evaluation of slowly growing cervical lymph nodes. He was diagnosed with grade II FL six years ago and was treated with four weekly rituximab three years ago. His lymph nodes are still relatively small, though they are becoming increasingly bothersome. He lives alone though he receives assistance from nearby family members.
Anti-CD20 monoclonal antibodies
The class I anti-CD20 monoclonal antibody rituximab revolutionized NHL treatment by improving outcomes in both the upfront and relapsed settings. Rituximab demonstrated an ORR of nearly 50% in patients with relapsed indolent lymphoma after four weekly intravenous doses of 375 mg/m2 (12). Improved outcomes were also seen with the addition of rituximab to chemotherapy combinations such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), and cyclophosphamide, vincristine, and prednisone (CVP) (13,14).
Our understanding of its efficacy and use in FL was furthered by the pivotal RESORT trial, which investigated rituximab maintenance compared to retreatment at the time of progression in patients with untreated low tumor burden FL. Disease control at the median follow-up of 4.5 years was similar between the two treatment strategies, demonstrating the utility of limited upfront treatment followed by rituximab retreatment at the time of progression. It is important to note that these strategies were utilized in patients with low tumor burden disease (15). Based on these data, repeated courses of rituximab can effectively be used in patients with low tumor burden FL with slow disease growth.
Additional anti-CD20 monoclonal antibodies such as obinutuzumab have shown promise in relapsed FL. Obinutuzumab is a novel glycoengineered humanized type II IgG1 anti-CD20 antibody. Compared to rituximab, obinutuzumab has more robust antibody-dependent cell-mediated cytotoxicity (ADCC) (16,17). The GAUSS study compared single-agent rituximab to obinutuzumab in patients with relapsed indolent lymphoma. In the FL cohort, ORR was higher in the patients treated with obinutuzumab compared to rituximab (44.6% vs. 26.7%). It is important to note that PFS was similar between the two groups and rates of infusion reactions were higher in patients receiving obinutuzumab (18).
Obinutuzumab has also been studied in combination with chemotherapy in the upfront and relapsed setting. The GADOLIN study investigated obinutuzumab plus bendamustine with obinutuzumab maintenance compared to bendamustine alone in relapsed FL. PFS was significantly prolonged in the obinutuzumab group compared to bendamustine alone at a median follow-up of 21.9 months (not reached vs. 14.9 months) (19). In the upfront setting, the GALLIUM investigated obinutuzumab based chemoimmunotherapy compared to rituximab based chemoimmunotherapy. Both groups received also received maintenance therapy. The obinutuzumab group had prolonged PFS at three years compared to the rituximab group (80% vs. 73.3%) (5).
Regardless of the specific anti-CD20 monoclonal antibody, retreatment at the time of progression has proven efficacy in low tumor burden disease. This strategy remains viable for patients with slowly progressing disease or those at advanced age or with significant comorbid conditions. Combination therapy is likely needed for patients with more aggressive or high tumor burden disease.
Clinical scenario 2
A 50-year-old woman presents with mild abdominal pain. She was diagnosed with grade I FL 4 years ago and was treated with rituximab for four weekly doses. PET imaging reveals widespread adenopathy with an abdominal mass around 7 cm in its most significant dimension and other enlarged lymph nodes ranging from 2–5 cm in size. Repeat biopsy confirms grade I FL.
Chemoimmunotherapy
For decades, chemotherapy has been the backbone of therapy for FL. This paradigm is now shifting toward a more novel and tailored approach. Despite these advances, chemoimmunotherapy remains an important option to provide rapid disease response and prolonged remission. Depending on the initial line of therapy, common chemotherapy agent(s) include bendamustine and cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab (CHOP) (20). When combined with anti-CD20 monoclonal antibodies, response rates in the relapsed setting often exceed 90%, with a median PFS near two years (21,22). While this article will not focus on chemotherapy agents, it must be recognized that they continue to have a notable role in relapsed FL. This is particularly for patients in early treatment stages and patients requiring a rapid disease response.
Immunomodulatory agents
Lenalidomide is an immunomodulatory (IMiD) agent that has efficacy across different forms of lymphoid malignancies in addition to specific subtypes of myelodysplastic syndrome (23-26). While the disruption of the ubiquitin-ligase cereblon with downregulation of Aiolos and Ikaros, has been eloquently described, further research has revealed anti-antiangiogenic effects along with alterations in T and NK cell function (27-29). T-cell function is of particular importance as FL cells have been shown to impair immunologic synapses furthering tumor growth and immune evasion. Lenalidomide can repair T-cell function in patients with FL providing a likely explanation for its efficacy in the disease (30,31).
Lenalidomide was studied as monotherapy in patients with relapsed and refractory indolent lymphomas, including those with FL. An initial study of 43 patients, including 22 with FL, revealed an overall response rate (ORR) of 23% with a median PFS of 4.4 months. Of the 22 patients with FL, six (27%) responded to therapy (32). Studies such as this revealed therapeutic efficacy with limited overall response and duration of response. To improve OS and PFS, clinical trials were quickly designed with the anti-CD20 monoclonal antibody rituximab and later with the class II anti-CD20 monoclonal antibody, obinutuzumab. In preclinical studies, the combinations were found to have synergistic effects secondary to improved ADCC and enhanced phagocytosis (33).
Improved efficacy of lenalidomide combined with rituximab compared to rituximab therapy alone in patients with relapsed indolent lymphomas was confirmed through the AUGMENT trial. At a median follow-up of 28 months, median PFS was 39.4 months with the combination compared to 14 months with lenalidomide alone. Results were similar between those patients who previously received bendamustine and rituximab (BR) and those who received cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab R-CHOP. ORR was 78% in the combination group compared to 53% in the lenalidomide alone group (25). The ongoing MAGNIFY trial is investigating maintenance strategies after 12 cycles of lenalidomide rituximab induction. Interim results have demonstrated a median PFS of 40 months with the 2.5-year treatment plan. The higher risk, more refractory group enrolled, likely explains the nearly identical PFS rates to those observed in AUGMENT (34). Efficacy with other anti-CD20 monoclonal antibody combinations was confirmed with obinutuzumab in the phase II GALEN trial. The combination of obinutuzumab and lenalidomide led to an ORR of 79% (35). Further combinations are being investigated, including lenalidomide and obinutuzumab with other agents affecting immune surveillance such as atezolizumab (36). Based on these trials, lenalidomide has been positioned as a key agent in the relapsed and refractory setting (6).
Compared to chemoimmunotherapy, lenalidomide requires daily by mouth administration for more extended treatment courses. Patient compliance is critical, which can be challenging, based not only on daily administration but also due to common side effects. In the AUGMENT study grade 3 or 4 neutropenia was experienced by 50% of patients taking lenalidomide and rituximab compared to only 13% of patients with rituximab alone. Outside of serious adverse events, side effects such as diarrhea, constipation, rash, headaches, and cough were more common in the lenalidomide combination. While events were grade 1 and 2, they can have important quality of life effects due to prolonged lenalidomide administration (25). While there are certainly challenges with the use of lenalidomide, based on favorable efficacy, it is an important option in relapsed FL.
Clinical scenario 3
A 62-year-old woman presents with progressive grade II FL. She was initially diagnosed 12 years ago and has thus far received three lines of therapy, including single-agent rituximab, BR, and most recently lenalidomide and rituximab. She is unable to travel, and no clinical trial options are available locally.
PI3K inhibitors
The phosphoinositide 3-kinase (PI3K) signaling pathway is critical to the survival and proliferation of B-cell lymphomas. While PI3K is expressed in several cell types throughout the body, the gamma and delta isoforms are concentrated in those of hematopoietic origin (37). Preclinical studies revealed that targeted small molecule inhibitors could limit the tonic expression of the B-cell receptor in lymphoma cell lines (38). Clinically, developed PI3K inhibitors have pronounced efficacy in indolent lymphomas, including FL. With the recent approval of umbralisib, four agents are currently approved for use in relapsed FL. The other approved PI3K inhibitors include idelalisib, duvelisib, and copanlisib (39-42).
Idelalisib was the first oral PI3K inhibitor developed and is highly specific to the delta isoform. The initial phase II study of idelalisib included 125 patients with indolent lymphomas, including 72 patients with FL who had disease refractory to rituximab and an alkylating agent. Based on an ORR of 56% with a median PFS of 11 months, idelalisib was approved (39). Further analyses identified that efficacy was similar in patients with high-risk characteristics such as those patients with early progression of disease (POD24) (43). Additional PI3K agents have been developed and approved for use, including duvelisib and copanlisib. duvelisib is an oral PI3K inhibitor with gamma and delta isoform activity, while copanlisib is an IV pan-class PI3K inhibitor. These agents have similar efficacy with an initial median ORR of 42% and 59% for duvelisib and copanlisib, respectively (40,41).
While there is apparent efficacy in relapsed FL, side effects of PI3K inhibitors have complicated their widespread use and made combination therapy challenging. Initial studies with idelalisib revealed pronounced inflammatory and infectious complications, including pneumonitis, colitis, hepatotoxicity, and severe infections. In a study of patients with chronic lymphocytic lymphoma (CLL), 54% of patients taking idelalisib combined with an anti-CD20 monoclonal antibody developed grade 3 or 4 hepatotoxicity (44). When combined with the spleen tyrosine kinase (SYK) inhibitor entospletinib, nearly 20% of patients developed grade 3 or higher pneumonitis (45). Grade 1 or 2 diarrhea and cough also occurred in 51.4% and 31.9% of patients with relapsed FL taking idelalisib monotherapy, respectively (39). Due to these complications, the FDA issued a black-box warning for the use of idelalisib, and several clinical trials were closed (46). One hypothesis for these observed toxicities is the suppression of normal T-regulatory cell function by PI3K inhibitors such as idelalisib (47). This knowledge has helped to explain prior toxicity and inform further clinical directions for PI3K inhibitors.
Due to variable isoform inhibition, side effects vary between the different agents. The most common adverse events for patients with indolent NHL receiving duvelisib monotherapy were diarrhea (48.8%), nausea (29.5%) and neutropenia (28.7%) (40). This side effect profile is comparable to idelalisib. Copanlisib has additional alpha isoform inhibition, which contributes to unique toxicities. These include hyperglycemia (57.1%) and hypertension (54.8%) with 23.5% and 40.5% being grade 3 or greater, respectively (41). Finally, the delta isoform PI3K inhibitor umbralisib was recently approved. In indolent NHL, umbralisib demonstrated an ORR of 45.3% and PFS of 10.6 months when used as monotherapy in patients with relapsed FL (42). Initial studies with umbralisib have recorded lower rates of inflammatory complications, including only 3% of patients developing grade 3 or higher pneumonia and 2% with the same grade colitis (48). Combination therapy with anti-CD20 monoclonal antibodies revealed lower rates of serious hepatotoxicity (4%) and diarrhea (8%) compared to prior PI3K inhibitor combinations (49).
The difference in rates of inflammatory toxicities between PI3K inhibitors may be due to differential PI3K isoform inhibition and differences in T-regulatory cell dysfunction (50). Beyond, the specific agent, toxicity may vary based due to patient characteristics such as number of prior lines of therapy and patient age. Studies has revealed high rates of inflammatory side effects in patients with untreated indolent lymphomas receiving PI3K inhibitor therapy. It is hypothesized that patients who have not received prior treatments have a more diverse and robust immune response leading to more the higher rates of inflammatory adverse effects such as diarrhea, pneumonitis and transaminitis (44,51,52).
With the expanding use of PI3K inhibitors in FL, strategies have been compiled to address toxicity management. Given the complexity of care, collaboration with other services such as gastroenterology and pulmonology can assist with rapid identification and management. As an example of management, diarrhea remains a common adverse event and expert opinion has been published for agents such as idelalisib and copanlisib (46,53). Proper identification and grading are critical to establish the need and timing of intervention. While differing between PI3K inhibitors, two different types of diarrhea have been identified including early onset and late onset. While early onset is often self-limiting, late-onset can be more severe and does not typically respond to conservative management.
For grade 1-2 (an increase of less than 6 stools per day over baseline), recommendations include an evaluation for alternative causes while maintaining the current dose of PI3K inhibitor. If no evidence of significant infection, loperamide can be used to help manage symptoms while recommending strategies to continue proper hydration. Proper reassessment is critical. If no improvement occurs, consideration of an oral or PO steroids could be considered as long as the diarrhea remains grade 2 or above. This is due to the fact that most cases of diarrhea will improve, though nonresponsive cases can progress quickly and should lead to discontinuation of the PI3K inhibitor with likely addition of steroids. With grade 3 or higher diarrhea, the PI3K inhibitor should be discontinued with rapid, often inpatient, follow-up. Other strategies have been developed for other inflammatory complications such as transaminitis and pneumonitis (54).
To improve treatment efficacy and safety, combination therapy along with alternative PI3K inhibitors have been investigated. For example, lower rates of inflammatory complications have been observed when PI3K inhibitors have been combined with agents that downregulate proinflammatory cytokine production, such as Janus kinase (JAK) inhibitors (55). A host of other PI3K inhibitors are currently in clinical development. Such agents include zandelisib (ME-401), parsaclisib (INCB050465), and bimiralisib (PQR-309) (56-59). PI3K inhibitors are an important tool in treating patients with relapsed FL though the duration of response is modest and toxicities are notable. For these reasons, PI3K inhibitors are not typically used in patients after their first disease relapse and are saved for later lines of therapy.
Tazemetostat
Tazemetostat is the most recently approved agent for use in relapsed FL. The histone methyltransferase, EZH2, is a critical enzyme in germinal center formation (60). Mutations of EZH2 lead to epigenetic silencing and proliferation of germinal centers with malignant clones (61). Analysis of B-cell lymphomas of germinal center origin, including FL, have demonstrated high rates of EZH2 mutations. EZH2 activating mutations are present in roughly 20% of patients with newly diagnosed and relapsed FL (62). Tazemetostat is first in its class. In phase I studies, including patients with relapsed B-cell lymphomas, side effects were tolerable with thrombocytopenia being the only dose-limiting toxicity. Most side effects were low grade, including anemia (14% of patients), nausea (20%), and asthenia (33%) (63).
A phase II study of tazemetostat included patients with FL refractory to at least two lines of therapy. Patients were stratified based on their EZH2 mutation status. ORR was 69% in the groups with EZH2 mutations and 35% in patients whose FL did not have an EZH2 mutation. The median PFS was 13.8 in patients with EZH2 mutated disease and 11.1 months in wild type disease. Grade three or higher adverse events included cytopenias; however, these were only present in four of 99 patients (64). Based on these results, tazemetostat received approval for use in patients who have an EZH2 mutation and have had at least two prior lines of therapy in addition to patients with FL who have no other alternative therapies available.
Tazemetostat provides another key option in patients with multiply relapsed FL. Given the different response rates for mutated and wild type patients, testing for EZH2 mutations is needed prior to use. To improve response rates and PFS, combination therapies are being studied, including the addition of lenalidomide and rituximab (NCT04224493).
Clinical scenario 4
A 45-year-old-man with grade IIIa FL presents with rapidly worsening symptoms. He was initially treated with R-CHOP therapy one year ago, however, now has worsening adenopathy, night sweats, and has lost 20 pounds. A biopsy is completed that demonstrates grade IIIa disease without evidence of large cell transformation.
Early relapsed FL
While most patients with FL will have long prolonged free intervals, a minority of patients will experience early progression of their disease after initial therapy. While there is no uniformly accepted definition, the disease progression within 24 months of treatment (POD24) has been increasingly used. Through analysis of The LymphoCare Study by Casulo et al., 20% of the 588 patients treated with upfront R-CHOP experienced progression of disease within 24 months of therapy. This subset of patients had inferior outcomes with a five-year OS of 50% compared to 90% in the group with disease progressing after two years (10). This finding was validated through a review of 13 large clinical trials and additionally in patients previously treated with upfront BR (65,66). Based on these findings, patients experiencing POD24 represent an unmet need in FL and an important group for clinical trial development.
Unfortunately, at present, there is no way to identify this group before early disease progression consistently. This is because a variety of patient and disease factors are likely involved in the progression of FL. Not only have increasing molecular differences been found at the time of relapse, but important changes to the tumor microenvironment and programmed cell death axis have also been described (67-69). Analysis of program cell death ligand 2 (PDL2) expression identified low expression as a poor risk factor and present in nearly 45% of patients experiencing POD24 (70). While out of this article’s scope, attempts have been made to combine biological and patient data to predict the risk of early progression.
Few large trials have been conducted to evaluate treatment for patients experiencing POD24 specifically. Several challenges make such studies difficult, including the rare occurrence of POD24 and its often-aggressive nature. That being said, several subset analyses of relapsed FL trials have been conducted. It is important to note that these studies often include patients refractory to prior chemotherapy. This section will focus mainly on novel approaches; however, if patients have not had prior anthracycline, CHOP-based regimens remain a reasonable approach. This is due to the fact that CHOP combined with an obinutuzumab can lead to response rates over 90% in patients with relapsed and refractory FL (22).
Beyond chemotherapy, subset analyses have been conducted, including patients with POD24 treated with agents such as obinutuzumab, lenalidomide, idelalisib, and tazemetostat. Overall, these studies have revealed the chemotherapy-resistant nature of early relapsed FL that many novel therapies may be able to overcome partially. The anti-CD20 monoclonal antibody obinutuzumab has proven to be an important backbone in many treatment regimens. In an evaluation of the GALLIUM study, there were fewer POD24 occurrences in patients receiving an obinutuzumab-based regimen compared to those receiving a rituximab-based regimen (5).
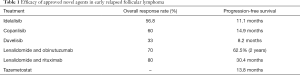
Lenalidomide has grown to be one of the favored options in relapsed FL. Analyses of both the GALEN and AUGMENT studies have revealed similar outcomes despite POD24 status. In the GALEN study 24 of the 86 patients were classified as having POD24, while 56 of the 147 patients receiving lenalidomide and rituximab had POD24 status. The Phase II GALEN trial studied obinutuzumab and lenalidomide in patients with relapsed FL and found an ORR of 70% and a median two-year PFS of nearly 63% in the POD24 group. This efficacy is similar to the study wide ORR and two-year PFS of 79% and 65%, respectively (35,71). These findings were further confirmed in the AUGMENT study involving rituximab and lenalidomide compared to rituximab in patients with relapsed indolent NHL. The response rate with lenalidomide and rituximab was nearly identical in both the POD24 and non-POD24 groups (71). Outside of lenalidomide, the efficacy of the PI3K agents idelalisib, copanlisib, and duvelisib, along with the EZH2 inhibitor tazemetostat, appear to be similar between POD24 and non-POD24 groups (Table 1) (40,43,64,72). A prospective clinical trial involving several of these drug classes is currently being conducted in patients with POD24 FL. S1608 involves three cohorts investigating obinutuzumab-based chemoimmunotherapy, lenalidomide obinutuzumab combination and the umbralisib obinutuzumab combination (NCT03269669).
Full table
Cellular therapies and immunologic strategies
Cellular therapies such as stem cell transplantation are utilized in patients with aggressive or multiply relapsed FL. Initial retrospective studies of patients with relapsed FL who underwent an ASCT revealed impressive outcomes, including a median PFS of almost 10 years with OS exceeding 20 years (21.3 years) (73). Such benefits were less robust in patients treated after their second complete remission (74). Other groups that may benefit from an early autologous transplant include those with early relapsed disease. An analysis of data from the LymphoCare study and the Center for International Blood and Marrow Transplant Research (CIMBTR) of patients experiencing early treatment failure demonstrated improved outcomes in patients who underwent an ASCT within one year of treatment failure compared to those who did not (five-year OS 73% vs. 60%) (75). An additional retrospective analysis revealed that outcomes were also improved in patients with early relapse undergoing an allogeneic stem cell transplant though patients experience higher rates of morbidity and mortality (76).
Beyond stem cell transplantation, other immunologic strategies including chimeric antigen receptor T-cell (CAR-T) therapy and bispecific antibodies have demonstrated promising results in clinical trials. The ZUMA-5 trial investigated axicabtagene cileulcel (axi-cel) in patients with relapsed and refractory FL. Response rates were over 90% with 80% of patients having a CR to therapy. Grade 3 or higher cytokine release syndrome (CRS) and neurotoxicity occurred in 11% and 19% of patients, respectively (77). Bispecific antibodies including odronextamab (REGN1979) and mosunetuzumab and others have efficacy in relapsed FL, including patients who previously received several lines of therapy including novel agents such as CAR-T therapy. Response rates for patients with relapsed FL receiving odronextamab and mosunetuzumab were 92.9% and 68%, respectively (78,79). It is expected that CAR-T therapy and bispecific antibodies will eventually become standard of care for patients with relapsed FL.
Conclusions
There is no uniformly accepted treatment strategy for patients with relapsed FL. Instead, the treatment landscape of relapsed FL is highly varied and must be tailored to the patient, considering treatment goals, disease biology, and relapse history. While chemoimmunotherapy combinations remain viable options, additional novel agents have established roles in therapy. When reasonable, clinical trials should be prioritized, as additional treatments such as antibody-drug conjugates, small molecular inhibitors, immunotherapies, bispecific antibodies, and CAR-T therapy promise to further expand our armamentarium (80-85). Further understanding of relapsed FL is critical to continue to prolong disease-free intervals and reduced treatment side effects.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Mark Roschewski, Carla Casulo) for the series “Follicular Lymphoma” published in Annals of Lymphoma. This article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aol-21-1). The series “Follicular Lymphoma” was commissioned by the editorial office without any funding or sponsorship. TDR reports that he has consulted for Targeted Oncology. PMB reports that he is consulting for Abbvie, Janssen, Genentech, Gilead, Morphosys, TG therapeutics, Seattle Genetics, BMS, Merck, MEI, Bayer, Astra Zeneca. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Teras LR, DeSantis CE, Cerhan JR, et al. 2016 US lymphoid malignancy statistics by World Health Organization subtypes. CA Cancer J Clin 2016;66:443-59. [Crossref] [PubMed]
- Tan D, Horning SJ, Hoppe RT, et al. Improvements in observed and relative survival in follicular grade 1-2 lymphoma during 4 decades: the Stanford University experience. Blood 2013;122:981-7. [Crossref] [PubMed]
- Brice P, Bastion Y, Lepage E, et al. Comparison in low-tumor-burden follicular lymphomas between an initial no-treatment policy, prednimustine, or interferon alfa: a randomized study from the Groupe d'Etude des Lymphomes Folliculaires. Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol 1997;15:1110-7. [Crossref] [PubMed]
- Luminari S, Ferrari A, Manni M, et al. Long-Term Results of the FOLL05 Trial Comparing R-CVP Versus R-CHOP Versus R-FM for the Initial Treatment of Patients With Advanced-Stage Symptomatic Follicular Lymphoma. J Clin Oncol 2018;36:689-96. [Crossref] [PubMed]
- Marcus R, Davies A, Ando K, et al. Obinutuzumab for the First-Line Treatment of Follicular Lymphoma. N Engl J Med 2017;377:1331-44. [Crossref] [PubMed]
- Morschhauser F, Fowler NH, Feugier P, et al. Rituximab plus Lenalidomide in Advanced Untreated Follicular Lymphoma. N Engl J Med 2018;379:934-47. [Crossref] [PubMed]
- Rummel MJ, Niederle N, Maschmeyer G, et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet 2013;381:1203-10. [Crossref] [PubMed]
- Montoto S, Davies AJ, Matthews J, et al. Risk and clinical implications of transformation of follicular lymphoma to diffuse large B-cell lymphoma. J Clin Oncol 2007;25:2426-33. [Crossref] [PubMed]
- Link BK, Maurer MJ, Nowakowski GS, et al. Rates and outcomes of follicular lymphoma transformation in the immunochemotherapy era: a report from the University of Iowa/MayoClinic Specialized Program of Research Excellence Molecular Epidemiology Resource. J Clin Oncol 2013;31:3272-8. [Crossref] [PubMed]
- Casulo C, Byrtek M, Dawson KL, et al. Early Relapse of Follicular Lymphoma After Rituximab Plus Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone Defines Patients at High Risk for Death: An Analysis From the National LymphoCare Study. J Clin Oncol 2015;33:2516-22. [Crossref] [PubMed]
- Noy A, Schöder H, Gönen M, et al. The majority of transformed lymphomas have high standardized uptake values (SUVs) on positron emission tomography (PET) scanning similar to diffuse large B-cell lymphoma (DLBCL). Ann Oncol 2009;20:508-12. [Crossref] [PubMed]
- McLaughlin P, Grillo-López AJ, Link BK, et al. Rituximab chimeric anti-CD20 monoclonal antibody therapy for relapsed indolent lymphoma: half of patients respond to a four-dose treatment program. J Clin Oncol 1998;16:2825-33. [Crossref] [PubMed]
- Hiddemann W, Kneba M, Dreyling M, et al. Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 2005;106:3725-32. [Crossref] [PubMed]
- Marcus R, Imrie K, Solal-Celigny P, et al. Phase III study of R-CVP compared with cyclophosphamide, vincristine, and prednisone alone in patients with previously untreated advanced follicular lymphoma. J Clin Oncol 2008;26:4579-86. [Crossref] [PubMed]
- Kahl BS, Hong F, Williams ME, et al. Rituximab Extended Schedule or Re-Treatment Trial for Low–Tumor Burden Follicular Lymphoma: Eastern Cooperative Oncology Group Protocol E4402. J Clin Oncol 2014;32:3096-102. [Crossref] [PubMed]
- Herter S, Herting F, Mundigl O, et al. Preclinical activity of the type II CD20 antibody GA101 (obinutuzumab) compared with rituximab and ofatumumab in vitro and in xenograft models. Mol Cancer Ther 2013;12:2031-42. [Crossref] [PubMed]
- Decaup E, Jean C, Laurent C, et al. Anti-tumor activity of obinutuzumab and rituximab in a follicular lymphoma 3D model. Blood Cancer J 2013;3:e131 [Crossref] [PubMed]
- Sehn LH, Goy A, Offner FC, et al. Randomized Phase II Trial Comparing Obinutuzumab (GA101) With Rituximab in Patients With Relapsed CD20+ Indolent B-Cell Non-Hodgkin Lymphoma: Final Analysis of the GAUSS Study. J Clin Oncol 2015;33:3467-74. [Crossref] [PubMed]
- Sehn LH, Chua N, Mayer J, et al. Obinutuzumab plus bendamustine versus bendamustine monotherapy in patients with rituximab-refractory indolent non-Hodgkin lymphoma (GADOLIN): a randomised, controlled, open-label, multicentre, phase 3 trial. Lancet Oncol 2016;17:1081-93. [Crossref] [PubMed]
- van Oers MHJ, Van Glabbeke M, Giurgea L, et al. Rituximab maintenance treatment of relapsed/resistant follicular non-Hodgkin's lymphoma: long-term outcome of the EORTC 20981 phase III randomized intergroup study. J Clin Oncol 2010;28:2853-8. [Crossref] [PubMed]
- Robinson KS, Williams ME, van der Jagt RH, et al. Phase II multicenter study of bendamustine plus rituximab in patients with relapsed indolent B-cell and mantle cell non-Hodgkin's lymphoma. J Clin Oncol 2008;26:4473-9. [Crossref] [PubMed]
- Radford J, Davies A, Cartron G, et al. Obinutuzumab (GA101) plus CHOP or FC in relapsed/refractory follicular lymphoma: results of the GAUDI study (BO21000). Blood 2013;122:1137-43. [Crossref] [PubMed]
- List A, Kurtin S, Roe DJ, et al. Efficacy of Lenalidomide in Myelodysplastic Syndromes. N Engl J Med 2005;352:549-57. [Crossref] [PubMed]
- Czuczman MS, Trněný M, Davies A, et al. A Phase 2/3 Multicenter, Randomized, Open-Label Study to Compare the Efficacy and Safety of Lenalidomide Versus Investigator's Choice in Patients with Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Clin Cancer Res 2017;23:4127-37. [Crossref] [PubMed]
- Leonard JP, Trneny M, Izutsu K, et al. AUGMENT: A Phase III Study of Lenalidomide Plus Rituximab Versus Placebo Plus Rituximab in Relapsed or Refractory Indolent Lymphoma. J Clin Oncol 2019;37:1188-99. [Crossref] [PubMed]
- Habermann TM, Lossos IS, Justice G, et al. Lenalidomide oral monotherapy produces a high response rate in patients with relapsed or refractory mantle cell lymphoma. Br J Haematol 2009;145:344-9. [Crossref] [PubMed]
- Gribben JG, Fowler N, Morschhauser F. Mechanisms of Action of Lenalidomide in B-Cell Non-Hodgkin Lymphoma. J Clin Oncol 2015;33:2803-11. [Crossref] [PubMed]
- Lopez-Girona A, Mendy D, Ito T, et al. Cereblon is a direct protein target for immunomodulatory and antiproliferative activities of lenalidomide and pomalidomide. Leukemia 2012;26:2326-35. [Crossref] [PubMed]
- Lu L, Payvandi F, Wu L, et al. The anti-cancer drug lenalidomide inhibits angiogenesis and metastasis via multiple inhibitory effects on endothelial cell function in normoxic and hypoxic conditions. Microvasc Res 2009;77:78-86. [Crossref] [PubMed]
- Ramsay AG, Clear AJ, Kelly G, et al. Follicular lymphoma cells induce T-cell immunologic synapse dysfunction that can be repaired with lenalidomide: implications for the tumor microenvironment and immunotherapy. Blood 2009;114:4713-20. [Crossref] [PubMed]
- Vo DN, Alexia C, Allende-Vega N, et al. NK cell activation and recovery of NK cell subsets in lymphoma patients after obinutuzumab and lenalidomide treatment. Oncoimmunology 2017;7:e1409322 [Crossref] [PubMed]
- Witzig TE, Wiernik PH, Moore T, et al. Lenalidomide oral monotherapy produces durable responses in relapsed or refractory indolent non-Hodgkin's Lymphoma. J Clin Oncol 2009;27:5404-9. [Crossref] [PubMed]
- Chiu H, Trisal P, Bjorklund C, et al. Combination lenalidomide-rituximab immunotherapy activates anti-tumour immunity and induces tumour cell death by complementary mechanisms of action in follicular lymphoma. Br J Haematol 2019;185:240-53. [Crossref] [PubMed]
- Lansigan F, Andorsky DJ, Coleman M, et al. Subgroup Analyses of Elderly Patients Aged ≥ 70 Years in MAGNIFY: A Phase IIIb Interim Analysis of Induction R2 Followed By Maintenance in Relapsed/Refractory Indolent Non-Hodgkin Lymphoma. Blood 2020;136:30-1. [Crossref]
- Morschhauser F, Le Gouill S, Feugier P, et al. Obinutuzumab combined with lenalidomide for relapsed or refractory follicular B-cell lymphoma (GALEN): a multicentre, single-arm, phase 2 study. Lancet Haematol 2019;6:e429-37. [Crossref] [PubMed]
- Morschhauser F, Ghosh N, Lossos I, et al. Efficacy and safety of obinutuzumab + lenalidomide + atezolizumab in patients with relapsed or refractory follicular lymphoma: primary analysis of a phase 1B/2 trial. Hematol Oncol 2019;37:113-4. [Crossref]
- Vanhaesebroeck B, Guillermet-Guibert J, Graupera M, et al. The emerging mechanisms of isoform-specific PI3K signalling. Nat Rev Mol Cell Biol 2010;11:329-41. [Crossref] [PubMed]
- Meadows SA, Vega F, Kashishian A, et al. PI3Kδ inhibitor, GS-1101 (CAL-101), attenuates pathway signaling, induces apoptosis, and overcomes signals from the microenvironment in cellular models of Hodgkin lymphoma. Blood 2012;119:1897-900. [Crossref] [PubMed]
- Salles G, Schuster SJ, de Vos S, et al. Efficacy and safety of idelalisib in patients with relapsed, rituximab- and alkylating agent-refractory follicular lymphoma: a subgroup analysis of a phase 2 study. Haematologica 2017;102:e156-9. [Crossref] [PubMed]
- Flinn IW, Miller CB, Ardeshna KM, et al. DYNAMO: A Phase II Study of Duvelisib (IPI-145) in Patients With Refractory Indolent Non-Hodgkin Lymphoma. J Clin Oncol 2019;37:912-22. [Crossref] [PubMed]
- Dreyling M, Santoro A, Mollica L, et al. Phosphatidylinositol 3-Kinase Inhibition by Copanlisib in Relapsed or Refractory Indolent Lymphoma. J Clin Oncol 2017;35:3898-905. [Crossref] [PubMed]
- Zinzani PL, Samaniego F, Jurczak W, et al. Umbralisib, the Once Daily Dual Inhibitor of PI3Kδ and Casein Kinase-1ε Demonstrates Clinical Activity in Patients with Relapsed or Refractory Indolent Non-Hodgkin Lymphoma: Results from the Phase 2 Global Unity-NHL Trial. Blood 2020;136:34-5. [Crossref]
- Gopal AK, Kahl BS, Flowers CR, et al. Idelalisib is effective in patients with high-risk follicular lymphoma and early relapse after initial chemoimmunotherapy. Blood 2017;129:3037-9. [Crossref] [PubMed]
- Lampson BL, Kasar SN, Matos TR, et al. Idelalisib given front-line for treatment of chronic lymphocytic leukemia causes frequent immune-mediated hepatotoxicity. Blood 2016;128:195-203. [Crossref] [PubMed]
- Barr PM, Saylors GB, Spurgeon SE, et al. Phase 2 study of idelalisib and entospletinib: pneumonitis limits combination therapy in relapsed refractory CLL and NHL. Blood 2016;127:2411-5. [Crossref] [PubMed]
- Coutré SE, Barrientos JC, Brown JR, et al. Management of adverse events associated with idelalisib treatment: expert panel opinion. Leuk Lymphoma 2015;56:2779-86. [Crossref] [PubMed]
- Chellappa S, Kushekhar K, Munthe LA, et al. The PI3K p110δ Isoform Inhibitor Idelalisib Preferentially Inhibits Human Regulatory T Cell Function. J Immunol 2019;202:1397-405. [Crossref] [PubMed]
- Burris HA 3rd, Flinn IW, Patel MR, et al. Umbralisib, a novel PI3Kδ and casein kinase-1ε inhibitor, in relapsed or refractory chronic lymphocytic leukaemia and lymphoma: an open-label, phase 1, dose-escalation, first-in-human study. Lancet Oncol 2018;19:486-96. [Crossref] [PubMed]
- Lunning M, Vose J, Nastoupil L, et al. Ublituximab and umbralisib in relapsed/refractory B-cell non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood 2019;134:1811-20. [Crossref] [PubMed]
- Maharaj KK, Powers JJ, Pabon-Saldana M, et al. Modulation of T Cell Compartment in a Preclinical CLL Murine Model By a Selective PI3K Delta Inhibitor, TGR-1202. Blood 2016;128:3236. [Crossref]
- Sharman JP, Coutre SE, Furman RR, et al. Final Results of a Randomized, Phase III Study of Rituximab With or Without Idelalisib Followed by Open-Label Idelalisib in Patients With Relapsed Chronic Lymphocytic Leukemia. J Clin Oncol 2019;37:1391-402. [Crossref] [PubMed]
- Rodgers TD, Williams AM, Baran A, et al. Toxicity patterns of novel PI3K combinations in patients with non-Hodgkin lymphoma. Leuk Lymphoma 2021;62:598-605. [Crossref] [PubMed]
- Cheson BD, O'Brien S, Ewer MS, et al. Optimal Management of Adverse Events From Copanlisib in the Treatment of Patients With Non-Hodgkin Lymphomas. Clin Lymphoma Myeloma Leuk 2019;19:135-41. [Crossref] [PubMed]
- Hanlon A, Brander DM. Managing toxicities of phosphatidylinositol-3-kinase (PI3K) inhibitors. Hematology 2020;2020:346-56. [Crossref] [PubMed]
- Hazem SH, Shaker ME, Ashamallah SA, et al. The novel Janus kinase inhibitor ruxolitinib confers protection against carbon tetrachloride-induced hepatotoxicity via multiple mechanisms. Chem Biol Interact 2014;220:116-27. [Crossref] [PubMed]
- Soumerai JD, Pagel JM, Jagadeesh D, et al. Initial results of a dose escalation study of a selective and structurally differentiated PI3Kδ inhibitor, ME-401, in relapsed/refractory (R/R) follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL). J Clin Oncol 2018;36:7519. [Crossref]
- Spriano F, Tarantelli C, Gaudio E, et al. Single and combined BTK and PI3Kδ inhibition with acalabrutinib and ACP-319 in pre-clinical models of aggressive lymphomas. Br J Haematol 2019;187:595-601. [Crossref] [PubMed]
- Tarantelli C, Gaudio E, Arribas AJ, et al. PQR309 Is a Novel Dual PI3K/mTOR Inhibitor with Preclinical Antitumor Activity in Lymphomas as a Single Agent and in Combination Therapy. Clin Cancer Res 2018;24:120-9. [Crossref] [PubMed]
- Phillips TJ, Corradini P, Gurion R, et al. Phase 2 Study Evaluating the Efficacy and Safety of Parsaclisib in Patients with Relapsed or Refractory Marginal Zone Lymphoma (CITADEL-204). Blood 2020;136:27-8. [Crossref]
- Margueron R, Reinberg D. The Polycomb complex PRC2 and its mark in life. Nature 2011;469:343-9. [Crossref] [PubMed]
- Béguelin W, Popovic R, Teater M, et al. EZH2 is required for germinal center formation and somatic EZH2 mutations promote lymphoid transformation. Cancer Cell 2013;23:677-92. [Crossref] [PubMed]
- Bödör C, Grossmann V, Popov N, et al. EZH2 mutations are frequent and represent an early event in follicular lymphoma. Blood 2013;122:3165-8. [Crossref] [PubMed]
- Italiano A, Soria JC, Toulmonde M, et al. Tazemetostat, an EZH2 inhibitor, in relapsed or refractory B-cell non-Hodgkin lymphoma and advanced solid tumours: a first-in-human, open-label, phase 1 study. Lancet Oncol 2018;19:649-59. [Crossref] [PubMed]
- Morschhauser F, Tilly H, Chaidos A, et al. Tazemetostat for patients with relapsed or refractory follicular lymphoma: an open-label, single-arm, multicentre, phase 2 trial. Lancet Oncol 2020;21:1433-42. [Crossref] [PubMed]
- Casulo C, Le-Rademacher J, Dixon J, et al. Validation of POD24 As a Robust Early Clinical Endpoint of Poor Survival in Follicular Lymphoma: Results from the Follicular Lymphoma Analysis of Surrogacy Hypothesis (FLASH) Investigation Using Individual Data from 5,453 Patients on 13 Clinical Trials. Blood 2017;130:412.
- Freeman CL, Kridel R, Moccia AA, et al. Early progression after bendamustine-rituximab is associated with high risk of transformation in advanced stage follicular lymphoma. Blood 2019;134:761-4. [Crossref] [PubMed]
- Kridel R, Chan FC, Mottok A, et al. Histological Transformation and Progression in Follicular Lymphoma: A Clonal Evolution Study. PLoS Med 2016;13:e1002197 [Crossref] [PubMed]
- Dave SS, Wright G, Tan B, et al. Prediction of survival in follicular lymphoma based on molecular features of tumor-infiltrating immune cells. N Engl J Med 2004;351:2159-69. [Crossref] [PubMed]
- Farinha P, Al-Tourah A, Gill K, et al. The architectural pattern of FOXP3-positive T cells in follicular lymphoma is an independent predictor of survival and histologic transformation. Blood 2010;115:289-95. [Crossref] [PubMed]
- Tobin JWD, Keane C, Gunawardana J, et al. Progression of Disease Within 24 Months in Follicular Lymphoma Is Associated With Reduced Intratumoral Immune Infiltration. J Clin Oncol 2019;37:3300-9. [Crossref] [PubMed]
- Leonard J, Trneny M, Izutsu K, et al. Augment phase III study: lenalidomide/rituximab (R2) improved efficacy over rituximab/placebo in relapsed/refractory follicular patients irrespective of POD24 status. Hematol Oncol 2019;37:114-5. [Crossref]
- Dreyling M, Santoro A, Leppä S, et al. Efficacy and safety in high-risk relapsed or refractory indolent follicular lymphoma patients treated with copanlisib. Hematol Oncol 2019;37:387-9. [Crossref]
- Jiménez-Ubieto A, Grande C, Caballero D, et al. Autologous Stem Cell Transplantation for Follicular Lymphoma: Favorable Long-Term Survival Irrespective of Pretransplantation Rituximab Exposure. Biol Blood Marrow Transplant 2017;23:1631-40. [Crossref] [PubMed]
- Kothari J, Peggs KS, Bird A, et al. Autologous stem cell transplantation for follicular lymphoma is of most benefit early in the disease course and can result in durable remissions, irrespective of prior rituximab exposure. Br J Haematol 2014;165:334-40. [Crossref] [PubMed]
- Casulo C, Friedberg JW, Ahn KW, et al. Autologous Transplantation in Follicular Lymphoma with Early Therapy Failure: A National LymphoCare Study and Center for International Blood and Marrow Transplant Research Analysis. Biol Blood Marrow Transplant 2018;24:1163-71. [Crossref] [PubMed]
- Smith SM, Godfrey J, Ahn KW, et al. Autologous transplantation versus allogeneic transplantation in patients with follicular lymphoma experiencing early treatment failure. Cancer 2018;124:2541-51. [Crossref] [PubMed]
- Jacobson CA, Chavez JC, Sehgal AR, et al. Interim analysis of ZUMA-5: A phase II study of axicabtagene ciloleucel (axi-cel) in patients (pts) with relapsed/refractory indolent non-Hodgkin lymphoma (R/R iNHL). J Clin Oncol 2020;38:8008. [Crossref]
- Assouline SE, Kim WS, Sehn LH, et al. Mosunetuzumab Shows Promising Efficacy in Patients with Multiply Relapsed Follicular Lymphoma: Updated Clinical Experience from a Phase I Dose-Escalation Trial. Blood 2020;136:42-4. [Crossref]
- Bannerji R, Allan JN, Arnason JE, et al. Odronextamab (REGN1979), a Human CD20 x CD3 Bispecific Antibody, Induces Durable, Complete Responses in Patients with Highly Refractory B-Cell Non-Hodgkin Lymphoma, Including Patients Refractory to CAR T Therapy. Blood 2020;136:42-3. [Crossref]
- Hirayama AV, Gauthier J, Hay KA, et al. High rate of durable complete remission in follicular lymphoma after CD19 CAR-T cell immunotherapy. Blood 2019;134:636-40. [Crossref] [PubMed]
- Nastoupil LJ, Westin JR, Fowler NH, et al. Response rates with pembrolizumab in combination with rituximab in patients with relapsed follicular lymphoma: Interim results of an on open-label, phase II study. J Clin Oncol 2017;35:7519. [Crossref]
- Advani R, Flinn I, Popplewell L, et al. CD47 Blockade by Hu5F9-G4 and Rituximab in Non-Hodgkin’s Lymphoma. N Engl J Med 2018;379:1711-21. [Crossref] [PubMed]
- Zinzani PL, Flinn IW, Yuen SLS, et al. Venetoclax-rituximab with or without bendamustine vs bendamustine-rituximab in relapsed/refractory follicular lymphoma. Blood 2020;136:2628-37. [PubMed]
- Advani RH, Flinn I, Sharman JP, et al. Two doses of polatuzumab vedotin (PoV, anti-CD79b antibody-drug conjugate) in patients (pts) with relapsed/refractory (RR) follicular lymphoma (FL): Durable responses at lower dose level. J Clin Oncol 2015;33:8503. [Crossref]
- Schuster SJ, Bartlett NL, Assouline S, et al. Mosunetuzumab Induces Complete Remissions in Poor Prognosis Non-Hodgkin Lymphoma Patients, Including Those Who Are Resistant to or Relapsing After Chimeric Antigen Receptor T-Cell (CAR-T) Therapies, and Is Active in Treatment through Multiple Lines. Blood 2019;134:6. [Crossref]
Cite this article as: Rodgers TD, Barr PM. Management of relapsed follicular lymphoma. Ann Lymphoma 2021;5:14.


